Archived News
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...

Matthew Lee, CPCRN co-Investigator | NYU-CUNY
...content is loading...
...content is loading...
...content is loading...
...content is loading...

...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...

...content is loading...

...content is loading...
...content is loading...
...content is loading...
...content is loading...

Austin Waters, CPCRN Scholar | University of North Carolina-Chapel Hill
...content is loading...
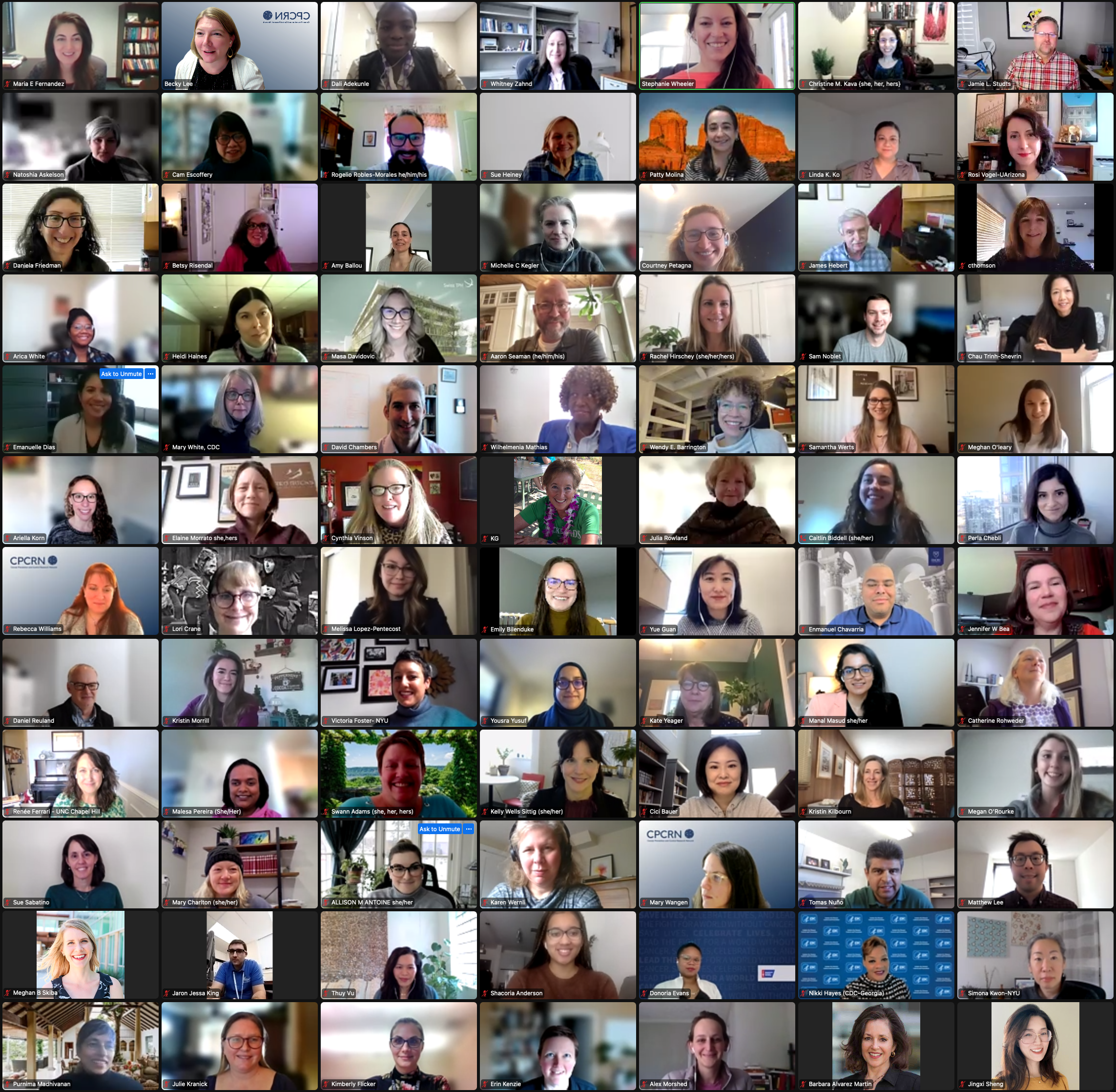
CPCRN5 Yr4 Virtual Winter Meeting Attendees | February 8, 2023
...content is loading...
...content is loading...
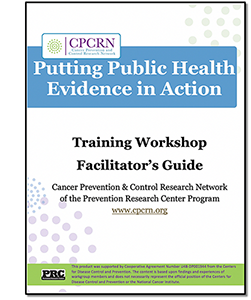
Cancer Screening Change Packages Currently Available for Breast, Cervical, and Colorectal Cancers
...content is loading...
...content is loading...
...content is loading...

Cam Escoffery, PhD, MPH, CHES | CPCRN Principal Investigator, Emory University
...content is loading...

Stephanie Wheeler, PhD, MPH, Principal Investigator, CPCRN Coordinating Center at UNC-Chapel Hill
...content is loading...

Rogelio Robles-Morales, MD, co-I (left); Kristin Morrill, PhD, co-I (right); Purnima Madhivanan, PhD, MBBS, MPH, co-I (bottom), University of Arizona
...content is loading...

Adriana Maldonado, PhD, MA, CPCRN Scholar, UofAZ (left); Yue Guan, PhD, ScM, co-I, Emory U (right); David O. Garcia, PhD, MS, FACSM, co-I, UofAZ (bottom)
...content is loading...

Jan Eberth, PhD, MSPH, affiliate member, Drexel University
...content is loading...

Rachel Issaka, MD, MAS | CPCRN co-investigator, University of Washington
...content is loading...

Ha Ngan (Milkie) Vu, PhD, MA (left), CPCRN Scholar, Northwestern University; Cam Escoffery, PhD, MPH, CHES (right), CPCRN Principal Investigator, Emory University
...content is loading...

Maria Fernández, PhD, MA, Affiliate Member, UTHealth Houston (left); David Chambers, DPhil, MSc, Federal Agency Partner, NCI (right)
...content is loading...
...content is loading...
...content is loading...

Whitney Zahnd, PhD, co-I, University of Iowa (left); Melinda Davis, PhD, CPCRN affiliate member, Oregon Health & Science University (right)
...content is loading...

Jennifer Leeman, DrPH, MPH, MDiv | co-Principal Investigator, University of North Carolina-Chapel Hill
...content is loading...

Emily Bilenduke, MA (left), CPCRN Project Director; Kristin Kilbourn, PhD (right), CPCRN co-I | Colorado School of Public Health
...content is loading...
...content is loading...
...content is loading...
Top: Sakhuja (left) & Noblet (right); Bottom: Drs. Wandersman (left) & Friedman (right)
...content is loading...

Prajakta Adsul, PhD, MBBS, MPH | Affiliate Member, UNM
...content is loading...

Lisa Spees, PhD, co-I, UNC (left); Stephanie Wheeler, PhD, MPH, Principal Investigator, CPCRN Coordinating Center at UNC (right)
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...

Jamie Studts, PhD, MA, MS | CPCRN co-investigator, Colorado School of Public Health
...content is loading...
...content is loading...

Sarah Nash, PhD | CPCRN Scholar, UI
...content is loading...

Sue Sabatino, MD (left); Mary C. White, ScD (right); & Lisa Richardson, MD (bottom) | Federal Agency Partners, CDC
...content is loading...

Maria E. Fernández, PhD | CPCRN Affiliate, UTHealth
...content is loading...

Aaron Scherer, co-I (left); Natoshia Askelson, PI (right) | University of Iowa
...content is loading...
...content is loading...
...content is loading...

Drs. Richard Hoffman (left), Barbara Baquero (right); Rima Afifi (bottom) | University of Iowa
...content is loading...

...content is loading...

...content is loading...

Abe Wandersman, PhD | co-I, USC
...content is loading...

Sarah Birken, PhD | Affiliate, Wake Forest School of Medicine
...content is loading...

...content is loading...

Dr. David Chambers | Federal Agency Partner, NCI
...content is loading...

Simona Kwon (left) & Nadia Islam (right) | co-Is, NYU-CUNY
...content is loading...

Jessica Islam, PhD | Affiliate, Moffitt Cancer Center
...content is loading...

Top (L to R): David Garcia, Kristin Morrill, Melissa Lopez-Pentecost; Bottom: Rosi Vogel, Cyndi Thomson, PI | UArizona
...content is loading...
...content is loading...

Betsy Risendal, PhD
...content is loading...

Daniela Friedman, PhD | co-PI, UofSC
...content is loading...

CPCRN Co-Author: Dr. Catherine Rohweder, co-PD at UNC
...content is loading...
Alison Brenner, PhD, co-PI (left) & Dan Reuland, MD, co-I (right) | UNC
...content is loading...
Noblet, MPH (left), Hébert, ScD (right), Friedman, PhD (center) | UofSC
...content is loading...
Top: Meghan O'Leary (L), Jennifer Leeman (R); Bottom: Dan Reuland (L); Stephanie Wheeler (R)
...content is loading...

(Left to right) Top: Ariella Korn, NCI; Shoba Ramanadhan, Harvard; Bottom: Thuy Vu, UW; April Oh, NCI
...content is loading...

*CPCRN Co-Authors: Tom Richards (left) & Lorna Thorpe (right)
...content is loading...

CPCRN Co-Author: Mary Charlton, PhD
...content is loading...
...content is loading...
...content is loading...

CPCRN Authors: Natoshia Askelson (left); Grace Ryan (right)
...content is loading...

Cyndi Thomson (top L); Tracy Crane (top R); David O. Garcia (bottom L); Linda Overholser (bottom R)
...content is loading...

CPCRN Co-Author: Sarah Birken, PhD
...content is loading...
...content is loading...

CPCRN Author: Prajakta Adsul, PhD
...content is loading...
...content is loading...
...content is loading...

CPCRN Co-Author: María Fernández
...content is loading...
...content is loading...
...content is loading...
CPCRN5 Year 3 Virtual Attendees
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...

CPCRN Co-Author: Linda Ko
...content is loading...

CPCRN Author: Robin Vanderpool
...content is loading...
...content is loading...
...content is loading...

CPCRN Authors: Prajakta Adsu (left)l; April Oh (right)
...content is loading...
...content is loading...

14th Annual (Virtual) D&I Conference
...content is loading...

Rebecca Williams, PhD, MHS | Chief Technology Officer/Co-I, CPCRN Coordinating Center
...content is loading...
...content is loading...

CPCRN Co-Author: Rachel Hirschey
...content is loading...
...content is loading...

Cici Bauer, PhD | CPCRN Affiliate, UTHealth
...content is loading...
...content is loading...
...content is loading...

Stephanie Wheeler, PhD, MPH | PI, CPCRN Coordinating Center
...content is loading...
...content is loading...

Prajakta Adsul, PhD, MPH, MBBS | CPCRN Affiliate, UNMCCC
...content is loading...
...content is loading...
...content is loading...

Simona Kwon, DrPH, MPH | co-I, NYU-CUNY Collaborating Center
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...

Rachel Hirschey, PhD, RN | CPCRN Co-Investigator, UNC
...content is loading...
...content is loading...

Dr. Sue Sabatino, CPCRN Federal Agency Partner of the CDC
...content is loading...

Drs. Mary Charlton (left) & Whitney Zahnd (right), CPCRN co-Is of the University of Iowa
...content is loading...

Dr. Purnima Madhivanan, CPCRN co-I of the University of Arizona
...content is loading...

Tatiana Enriquez, CPCRN co-I of the University of Arizona
...content is loading...
...content is loading...
...content is loading...

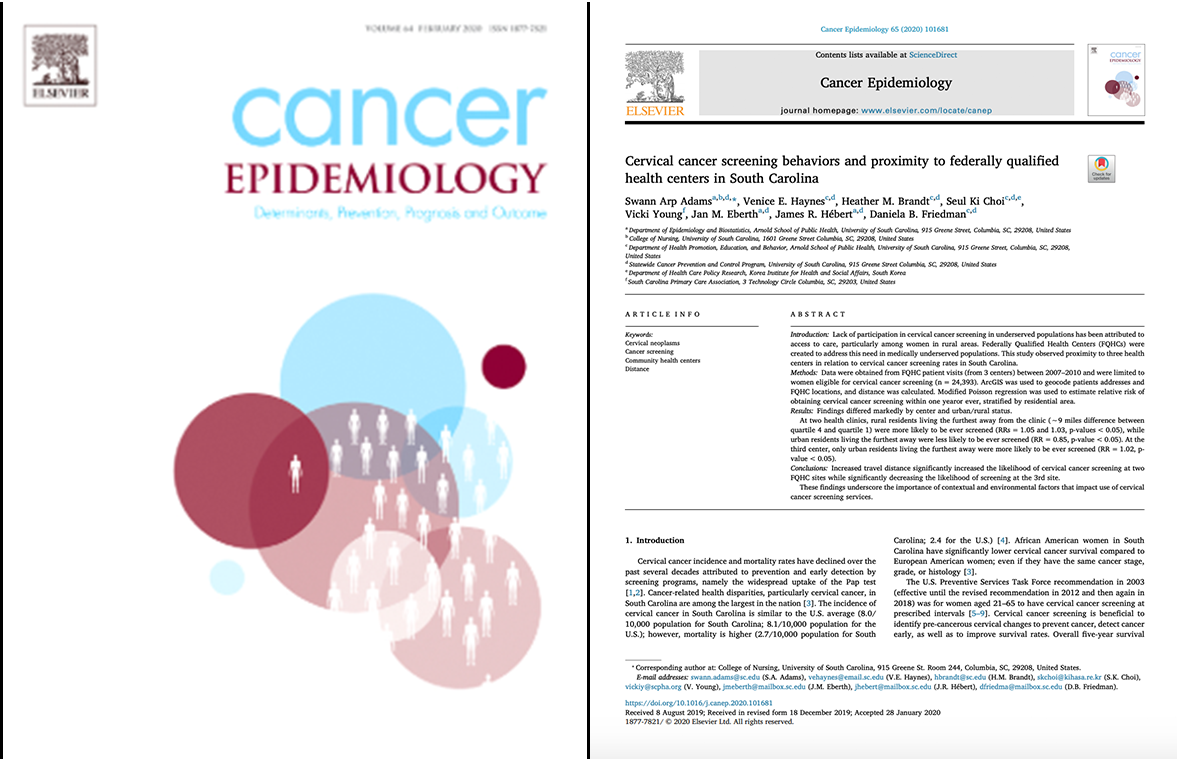
Friedman et al., July 2021
...content is loading...
...content is loading...

Robin Vanderpool, DrPH, Federal Agency Partner of the NCI
...content is loading...

Dr. Sarah Birken, CPCRN affiliate, Wake Forest School of Medicine
...content is loading...
...content is loading...

Dr. Sarah Birken, CPCRN Affiliate of the Wake Forest School of Medicine
...content is loading...

Dr. Heidi Hamann, CPCRN co-investigator of the University of Arizona
...content is loading...
...content is loading...

Dr. Shoba Ramanadhan, CPCRN affiliate of the Harvard School of Public Health
...content is loading...

...content is loading...

Dr. Maria Fernandez, CPCRN affiliate of UTHealth
...content is loading...

Jessica Islam, PhD, MPH, CPCRN Scholar 2020-'21
...content is loading...

Dr. Chau Trinh-Shevrin, CPCRN PI of NYU-CUNY
...content is loading...

Dr. Bryan Weiner, CPCRN co-I of the University of Washington
...content is loading...
...content is loading...

Dr. Sue Heiney, CPCRN co-I of the University of South Carolina
...content is loading...
...content is loading...

Melissa Lopez-Pentecost, MS
...content is loading...

Dr. Arica White, CPCRN Federal Agency Partner of the CDC
...content is loading...
...content is loading...
...content is loading...

Dr. Shannon Watkins, co-I of the University of Iowa
...content is loading...
...content is loading...
...content is loading...
...content is loading...

Dr. Robin Vanderpool, CPCRN Federal Agency Partner of the NCI
...content is loading...

CPCRN Scholars Program, Inaugural Cohort Members
...content is loading...
...content is loading...

Purnima Madhivanan, PhD, MPH, MBBS, co-I of UAz Collaborating Center
...content is loading...

...content is loading...
...content is loading...
...content is loading...
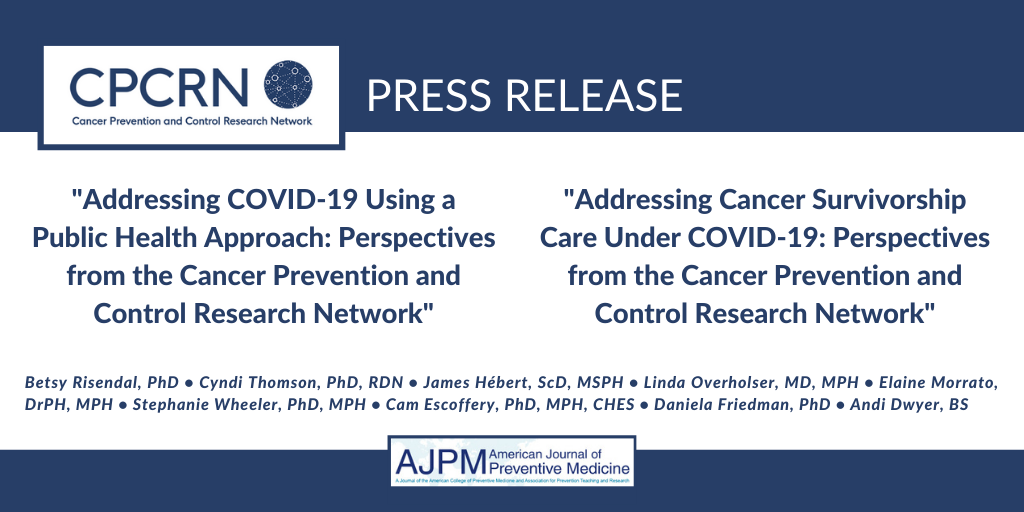
CPCRN Sister Articles, AJPM, Apr 2021
...content is loading...

Chau Trinh-Shevrin, DrPH, CPCRN PI of the NYU-CUNY Collaborating Center
...content is loading...

Robert Bednarczyk, PhD, CPCRN co-I of Emory University
...content is loading...

Daniela Friedman, PhD, co-PI of USC Collaborating Center
...content is loading...

Dr. Sarah Birken, CPCRN affiliate of the Wake Forest School of Medicine
...content is loading...

...content is loading...
...content is loading...

Stephanie Wheeler, PhD, MPH, PI of the CPCRN Coordinating Center
...content is loading...

Mary Charlton, PhD, MS, co-I of UIowa Collaborating Center
...content is loading...

Jan Eberth, PhD, CPCRN co-I of USC
...content is loading...
...content is loading...
...content is loading...

...content is loading...
...content is loading...

Drs. Nadia Islam, co-I (left) & Chau Trinh-Shevrin, PI (right) | NYU-CUNY
...content is loading...

Dr. Mary Charlton, CPCRN co-I of the University of Iowa
...content is loading...
...content is loading...
...content is loading...

Allison Cole, MD, MPH, CPCRN co-I of UW Collaborating Center
...content is loading...

Purnima Madhivanan, PhD, MPH, MBBS, co-I of UAz CPCRN Center
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...

Stephanie Wheeler, PhD, MPH, PI of the UNC Coordinating Center
...content is loading...

...content is loading...
...content is loading...

Jennifer Leeman, DrPH, MPH, MDiv, CPCRN co-PI of UNC Collaborating Center
...content is loading...

Sue Heiney, PhD, RN, FAAN, co-I of USC, presents inaugural award to MD Anderson Cancer Center
...content is loading...
...content is loading...
...content is loading...

David Chambers, DPhil, MSc, Federal Agency Partner of the NCI
...content is loading...

Virtual attendees at the CPCRN5 Year 2 Annual Meeting
...content is loading...
...content is loading...

Alison Brenner, PhD, MPH, Co-Principal Investigator of UNC
...content is loading...

Lead author, Whitney Zahnd, PhD, co-I of USC
...content is loading...

...content is loading...

Mary C. White, ScD, Federal Agency Partner, CDC
...content is loading...

Susan Sabatino, MD, MPH, Federal Agency Partner, CDC
...content is loading...

David Chambers, DPhil, MSc (left) & Wynne Norton, PhD (right), Federal Agency Partners of the NCI
...content is loading...

Andrea Dwyer, CPCRN co-I of the Colorado School of Public Health
...content is loading...
...content is loading...

Sarah Birken, PhD, MSPH, Affiliate, Wake Forest University
...content is loading...
...content is loading...

Cynthia Thomson, PhD, RDN, FTOS, PI of University of Arizona
...content is loading...

David O. Garcia, PhD, FACSM, co-investigator of the University of Arizona
...content is loading...

Cam Escoffery, PhD, MPH, CHES, PI of Emory University
...content is loading...

Jennifer Leeman, DrPH, MPH, MDiv, Principal Investigator (left) & Victoria Petermann, BSN, RN (right) of UNC
...content is loading...

Heather Brandt, PhD, MSPH, Affiliate of St. Jude Children's Research Hospital
...content is loading...

Whitney Zahnd, PhD, co-investigator, University of South Carolina
...content is loading...

...content is loading...

Top: Drs. Zahnd (left), Adams (right); and Bottom: Drs. Eberth (left), Brandt (right)
...content is loading...
...content is loading...
...content is loading...

Allison Cole, MD, MPH co-investigator of the University of Washington
...content is loading...

Swann Arp Adams, PhD, MS, FACE, co-investigator of the University of South Carolina
...content is loading...

Stephanie Wheeler, PhD, MPH, PI of CPCRN Coordinating Center (left); Sarah Birken, PhD, MSPH, affiliate of Wake Forest University
...content is loading...

...content is loading...

Kate Yeager, PhD, RN, MS, co-investigator, Emory Unviersity
...content is loading...

Jennifer Leeman, DrPH, MPH, MDiv, Co-PI (left) & Catherine Rohweder, DrPH, Co-PD (right) of UNC
...content is loading...

...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...

Dr. Shannon Watkins, co-I | University of Iowa
...content is loading...

Gila Neta, PhD, MPP, federal agency partner of the NCI
...content is loading...
...content is loading...

Robin Vanderpool, DrPH, federal agency partner of the NCI
...content is loading...

Rachel Hirschey, PhD, RN, co-I of UNC CPCRN Collaborating Center
...content is loading...
...content is loading...
...content is loading...

Mary Charlton, PhD, MS, co-investigator of UI
...content is loading...
...content is loading...

...content is loading...
...content is loading...

...content is loading...

...content is loading...
...content is loading...

...content is loading...

...content is loading...

...content is loading...

...content is loading...

Jan Eberth, PhD, Co-Investigator, University of South Carolina
...content is loading...

Rosi Vogel, BBA/MBA (left) & David O. Garcia, PhD, FACSM (right), University of Arizona
...content is loading...

Mary Charlton, PhD (left), Nicole Novak, PhD (center), Aaron Scherer, PhD (right)
...content is loading...

...content is loading...

David Chambers, DPhil, MSc, National Cancer Institute
...content is loading...

...content is loading...

...content is loading...

Daniela Friedman, PhD, Principal Investigator, University of South Carolina
...content is loading...

Sue Heiney, PhD, RN, FAAN, co-investigator, University of South Carolina
...content is loading...

Russell Glasgow, PhD, co-investigator, Colorado School of Public Health
...content is loading...
...content is loading...

David Chambers, DPhil, MSc, NCI Federal Agency Partner
...content is loading...
...content is loading...
...content is loading...

Sarah Birken, PhD, MPSH, Affiliate, Wake Forest University
...content is loading...

Robin Vanderpool, DrPH, Federal Agency Partner of NCI
...content is loading...
...content is loading...

Dr. David Chambers (left) and Dr. Wynne Norton (right)
...content is loading...
...content is loading...
...content is loading...
...content is loading...
Dr. Natoshia Askelson (left), Dr. Aaron Scherer, (center), & Dr. Rima Afifi (right)
...content is loading...

Jan Eberth, PhD, co-investigator of the University of South Carolina
...content is loading...

Cam Escoffery, PhD, MPH, CHES, PI of Emory University
...content is loading...

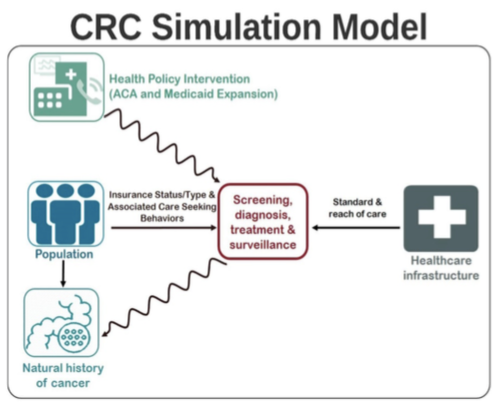
Trogdon and Wheeler
...content is loading...
CPCRN federal agency partners of NCI, April Oh, PhD, MPH (left), Cynthia Vinson, PhD, MPA (center), and David Chambers, DPhil, MSc (right)
...content is loading...

...content is loading...

Whitney Zahnd, PhD, co-investigator of the University of South Carolina
...content is loading...

...content is loading...

...content is loading...
...content is loading...
...content is loading...

University South Carolina CPCRN investigators design a virtual slide to recognize and celebrate Dr. Brandt
...content is loading...
...content is loading...

Dr. Eberth selected as National Rural Health Assoc. Outstanding Researcher
...content is loading...
...content is loading...

...content is loading...

Sarah Birken, PhD, MSPH, University of North Carolina
...content is loading...
...content is loading...

CPCRN researchers at the Jan. 27-28 kickoff meeting in Chapel Hill, N.C.
...content is loading...

Jennifer Leeman, DrPH, MDiv (left), Catherine Rohweder, DrPH (center), Mary Wangen, MPH (right)
...content is loading...

Rebecca Williams, PhD, MHS, University of North Carolina
...content is loading...

...content is loading...

Shannon Watkins, PhD, University of Iowa
...content is loading...

Jan Eberth, PhD & Whitney Zahnd, PhD, University of South Carolina
...content is loading...

Daniela Friedman, PhD (left) & Heather Brandt, PhD (right)
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...

...content is loading...
...content is loading...

...content is loading...
...content is loading...

...content is loading...
...content is loading...

...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
Karen Glanz, PhD, PI of the UPenn Collaborating Center
...content is loading...

Erika Trapl, PhD, CWRU
...content is loading...

Stephanie Wheeler, PhD, PI of the CPCRN Coordinating Center
...content is loading...

Cam Escoffery, PhD, CPCRN Affiliate of Emory University
...content is loading...

...content is loading...
...content is loading...
...content is loading...

Robin Vanderpool, DrPH, PI of UK CPCRN Collaborating Center
...content is loading...

Jennifer Leeman, DrPH, PI of the UNC CPCRN Collaborating Center
...content is loading...
...content is loading...

...content is loading...
...content is loading...

Karen Glanz, PhD, PI of the UPenn CPCRN Collaborating Center
...content is loading...
...content is loading...

...content is loading...
...content is loading...
...content is loading...
...content is loading...

...content is loading...

...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...

...content is loading...
...content is loading...
...content is loading...
...content is loading...

...content is loading...
...content is loading...
...content is loading...

...content is loading...
...content is loading...
...content is loading...

Jennifer Leeman, DrPH
...content is loading...

...content is loading...

...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...
...content is loading...

...content is loading...

...content is loading...

...content is loading...
...content is loading...
...content is loading...
...content is loading...



